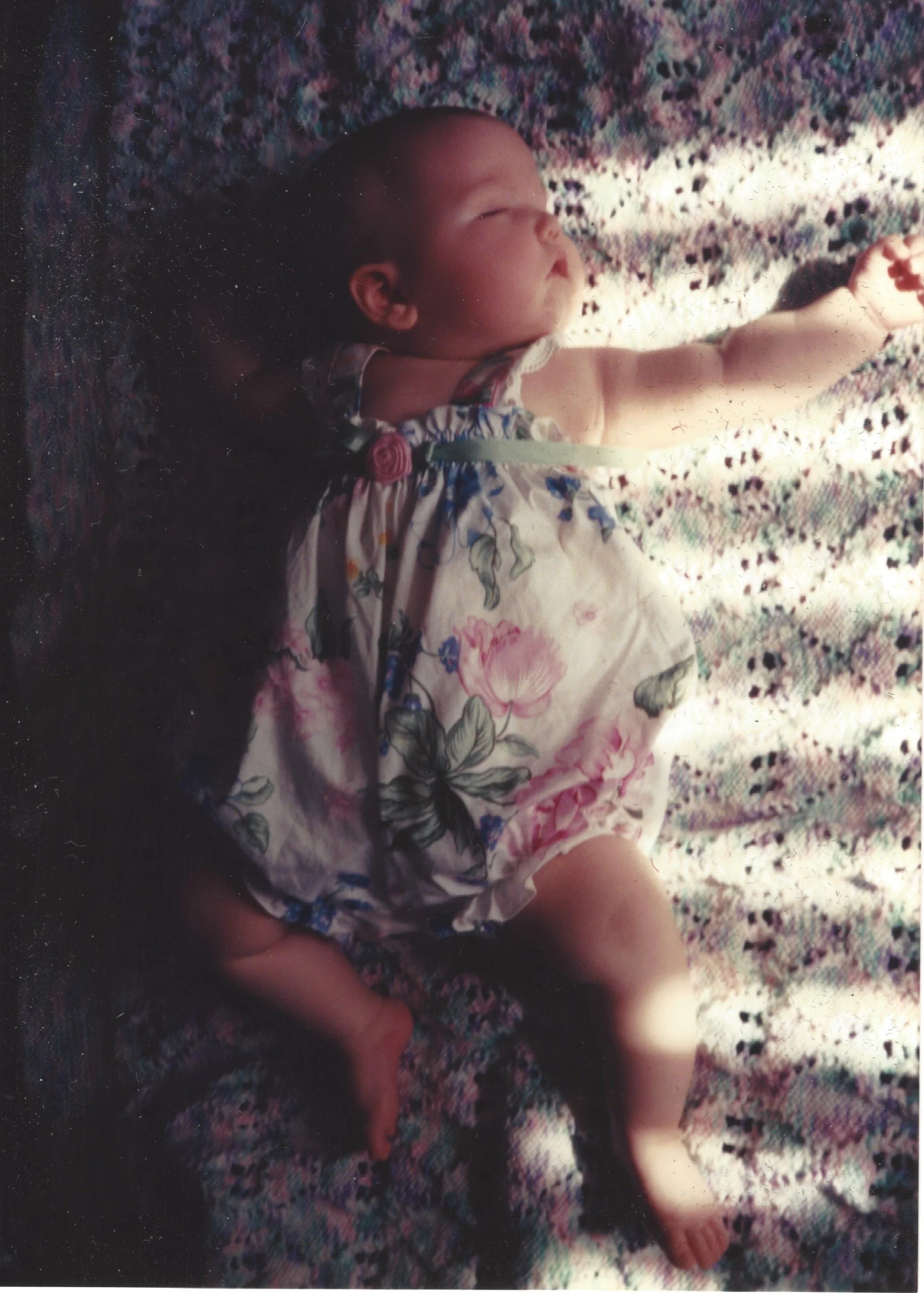
I am just publishing an essay collection with my friend and colleague Luigi Manca on the subject of global environmental health and welfare and the media -- Interdisciplinary Essays on Environment and Culture: One Planet, One Humanity and the Media -- and I am also currently at work on a monograph on environmental chemical and childhood health. Honestly, I would predict that the greatest threat to public health globally in the long run is climate change. But the second greatest, and one that likely harms more people right now, is environmental contamination with toxic chemicals. A subset of that problem, one that ruined my own life by causing the leukemia that killed my first-born child, is global contamination with toxic pesticides. First, a definition: pesticide is a term that encompasses chemicals used to kill a variety of pests, including insecticides, herbicides, fungicides, and rodenticides. This is appropriate because many of these chemicals – those applied to lawns, for instance – are used in combination. Studies showing links between childhood cancer and pesticides began steadily filling the primary literature in the late 1970s, and the topic was never entirely neglected by the popular media (Fabia & Thuy 1974; Gold et al. 1979; Infante & Newton 1975; Pratt et al. 1977; Reeves 1982). Pesticides in combination, as we encounter them in the environment, are 10 to 1000 times more toxic than they are singly, as they are tested, if they are tested at all (Arnold et al. 1996). Studies show that most of the pesticide exposure babies have is through their food (Amaroli et al. 2013). The President’s Cancer Panel, one of the most authoritative summaries of the research, reiterates some of these cautions: “registered pesticides contain nearly 900 active ingredients, many of which are toxic. Many of the inert ingredients in pesticides also are toxic, but are not required to be tested for causing chronic diseases such as cancer. For example, xylene is used as the inert ingredient in almost 900 pesticides and has been associated with increased risk of brain tumors, rectal cancer, and leukemia” (PCP 2010). Such testing as is done is almost all voluntary and most often done by those with an economic interest in the chemicals, the pesticide manufacturers themselves.[1]
A few review articles summarize the research of the last twenty years or so, and they all find that the preponderance of evidence shows a significant link between exposure to pesticides and childhood cancer, particularly brain tumors and acute lymphocytic leukemia (ALL). The keystone of the research on pesticides and childhood cancer is Zahm and Ward’s 1998 review, and then Claire Infante-Rivard and Scott Weichenthal’s update to Zahm and Ward in 2007. In 1998, there was already abundant, decades-long evidence for the link between pesticides and childhood cancer. Zahm and Ward noted that the effect of these chemicals on children was much more significant than the effect seen in adults, because children are more sensitive to the exposures and have lower body weights. They reviewed 112 articles, and the great majority of them showed higher levels of various childhood cancers with exposure to pesticides. This was the case even though children are immersed in a soup of toxic chemicals of all kinds from conception onwards; the fact that a correlation between cancer and pesticides in particular was found at all is a remarkable scientific accomplishment when you consider that there is no control group, no group unexposed to pesticides and tens of thousands of other chemicals.
Zahm and Ward describe how children are exposed, because after all, very few parents intend to expose their children to toxic chemicals. The fact that children are exposed and have testable levels of pesticides in their bodies is an important finding in and of itself because in the past, pesticide manufacturers, regulators, and users have all assumed that pesticides can be kept separate from ourselves with appropriate precautions. That is not the case. Pesticides are used in pest strips, pet flea treatments, garden chemicals, and indoor products that purport to be safe. Pesticides drift into homes and yards from agricultural or landscape applications. Pesticides are tracked inside from lawn treatments, are transported home by parents, or are transferred from pets to children. Once indoors, pesticides adhere to dust particles, on the floor and in the carpet where children are constantly crawling and laying, moving hands to mouths, as babies and children naturally and inevitably do.
Water sources are nearly universally contaminated with varying levels of pesticides: “A 1994 study of tests for five herbicides in 20,000 samples of tap water and drinking water sources found that 14.1 million people routinely drink water contaminated with atrazine, cyanazine, simazine, alachlor, and metolachlor” (Zahm and Ward 1998). Many people are drinking two or more of these on a regular basis. Pesticides remain in the groundwater, even if the land has not been chemically treated in years, even decades (Kloos 1996; UC Berkeley 1995). One study found that one in five peaches exposed children to dangerous levels of organophosphates (Wiles et al. 1998). Another study found a lethal potato, with levels of aldicarb that could kill an adult (Physicians 1995). This shows the haphazard high exposures individuals can encounter, just as a matter of chance, though most estimates of risk are based on average exposures. At the time Zahm and Ward wrote, 84% of homes used pesticides inside, while common outdoor pesticide applications, organophosphates for termite control, for example, often found their way indoors.
Many of these studies are case control studies, where sick children are matched with children like them in every regard except for disease status, and their exposures compared. The hypothesis is that sick children will have been exposed to more environmental chemicals than well children like them. Zahm and Ward acknowledged some limitations in studies at the time: the lack of studies looking at specific pesticides and the possibility of recall bias, where parents of sick children are more likely to recall toxic exposures than parents of well children because they are more aware, a potential flaw that many subsequent studies are now helping to address in various ways. These more recent studies have defended the assumptions and validity of the previous methods by showing, for instance, that exposures reported by parents correlate reliably with actual measures of chemical body burden, carpet dust, or biomarkers of exposure (Metayer et al. 2008; Rudant et al. 2010; Costa et al. 2011; Slusky et al. 2012). It turns out that the concerns about recall bias did not amount to much in the end. Dr. Aaron Blair, whom I personally interviewed about this, says that, “though we should worry about it, I don’t actually think it occurs very often, even in the case control studies. It can’t happen in the cohort study, and I don’t think it even happens very much in the case control. We did a little methodological study and found no evidence whatsoever of recall bias. What does happen is exposure misclassification, and it happens in spades.” And this flaw, along with others of the flaws with these studies, would tend to underestimate, not overestimate, the risk of cancer.[2] They call this a bias toward the null, or a propensity not to find a connection between disease and exposure when one really exists. As with climate change, people tend not to think about science being wrong in the wrong direction; things could be worse than the most current science represents, not better.
Overall, Zahm and Ward found links between all the above childhood cancers and higher exposures to pesticides. Exposure to pesticides, even one year before conception, was linked to a two-fold increased risk of acute leukemia (Meinert et al. 1996; Meinert et al. 2000; Infante-Rivard et al. 1999; Ma et al. 2002; VanMaele-Fabry et al. 2011). In plain English, we have been systematically poisoning our children for decades, and we knew it all along. We have been just too cowardly to face this terrible truth.
What could be done? Plenty. A good start would be regulating pesticides more strictly, both in the U.S. and worldwide. The E.U. already has more stringent regulations. The Toxic Substance Control Act, currently the only real regulation, is so weak that only six substances out of the tens of thousands of toxic chemicals have very been banned, and the ban on asbestos was overturned in court. Frank Lautenberg has introduced a bill to congress called the Frank R. Lautenberg Chemical Safety for the 21st Century Act (S. 697), which while not perfect, would do much to improve chemical safety in this country. I will be sending a version of this to my Senators using The Environmental Defense Fund’s activist page and personalizing the email, and I urge everyone reading this to do the same. Before we can begin to address this problem globally, we must get our own house in order, and this would be a good step in that direction.
References
Amaroli, A., Aluigi, M.G., Falugi, C., & Chessa, M.G. (2013). Effects of the neurotoxic thionophosphate pesticide chlorpyrifos on differentiating alternative models. Chemosphere 90: 2115-22
Arnold SF, Klotz DM, Collins BM, Vonier PM, Guilette LJ, McLachlan JA. 1996. Synergistic activation of estrogen receptor with combinations of environmental chemicals. Science 272:1489-1492.
Blair A, Thomas K, Coble J, Sandler DP, Hines CJ, Lynch CF, Knott C, Purdue MP, Zahm SH, Alavanja MCR, Dosemeci M, Kamel F, Hoppin JA, Freeman LB, Lubin JH. 2011. Impact of pesticide exposure misclassification on estimates of relative risks in the Agricultural Health Study 68(7):537-541.
Costa C, Silva S, Neves J, Coelho P, Costa S, Laffon B, Snawder J, Teixeira JP. 2011. Micronucleus frequencies in lymphocytes and reticulocytes in a pesticide-exposed population in Portugal. J Toxicology and Environ Health, Part A 74:960-970.
Fabia, J., Thuy, T.D. (1974). Occupation of father at time of birth of children dying of malignant diseases. Br J Prey Soc Med 28:98-100.
Gold, E., Gordis, L., Tonascia, J., Szklo, M. (1979). Risk factors for brain tumors in children. Am J Epidemiol 109, 309-319.
Infante, P.F., Newton, W.A., Jr. (1975). Letter: Prenatal chlordane exposure and neuroblastoma. N Engl J Med 293(6), 308–308.
Infante-Rivard C, Labuda D, Krajinovic M, Sinnett D. 1999. Risk of childhood leukemia associated with exposure to pesticides and with gene polymorphisms. Epidemiology10(5):481–7.
Kloos H. 1996. 1,2 Dibromo-3-chloropropane (DBCP) and ethylene dibromide (EDB) in well water in the Fresno/Clovis metropolitan area, California. Arch Environ Health 51:291-299.
Ma X, Buffler PA, Gunier RB, Dahl G, Smith MT, Reinier K, Reynolds P. 2002. Critical windows of exposure to household pesticides and risk of childhood leukemia. Environ Health Perspect 110(9):955-960.
Meinert R, Kaatsch P, Kaletsch U, Krummenauer F, Miesner A, Michaelis J. 1996. Childhood leukaemia and exposure to pesticides: Results of a case-control study in northern Germany. Eur J Cancer 32A:1943–1948.
Meinert R, Schüz J, Kaletsch U, Kaatsch P, Michaelis J. 2000. Leukemia and Non-Hodgkin’s Lymphoma in childhood and exposure to pesticides: Results of a register-based case-control study in Germany. Epidemiology 151(7):639-646.
Metayer C, Buffler PA. 2008. Residential exposures to pesticides and childhood leukaemia. Radiat Prot Dosim 132(2):212–9.
Physicians for Social Responsibility. 1995. Pesticides and Children: What the Pediatric Practitioner Should Know. Washington: Physicians for Social Responsibility: 1-8.
Pratt CB, Rivera G, Shanks E, Johnson WW, Howarth C, Terrell W, Kumar APM. 1977. Colorectal carcinoma in adolescents: implications regarding etiology. Cancer 40:2464-2472.
President’s Cancer Panel (PCP). 2010. Reducing environmental cancer risk: What we can do now. U.S. Department of Health and Human Services. Available at http://deainfo.nci.nih.gov/advisory/pcp/annualReports/pcp08-09rpt/PCP_Report_08-09_508.pdf
Reeves JD. 1982. Household insecticide-associated blood dyscrasias in children. Am J Hematol Oncol 4:438-439.
Rudant J, Clavel J, Infante-Rivard C. 2010. Selection bias in case-control studies on household exposure to pesticides and childhood acute leukemia. J Exposure Science Environ Epidemiology 20(4):299-309.
Slusky DA, Metayer C, Aldrish MC, Ward MH, Lea CS, Selvin S, Buffler PA. 2011. Reliability of maternal-reports regarding the use of household pesticides: Experience from a case-control study of childhood leukemia. Cancer Epidemiology 36:375-80.
University of California Berkeley School of Public Health. 1995. Pesticide Contamination of Groundwater in California. Berkeley CA: University of California.
U.S. EPA. 2013. Test guidelines for data requirements. USEPA. Available at http://www.epa.gov/pesticides/science/guidelines.htm
Van Maele-Fabry G, Lantin A-C, Hoet P, Lison D. 2011. “Residential exposure to pesticides and childhood leukaemia: A systematic review and meta-analysis. Environment International 37:280-291.
Wiles R, Davies K, Campbell C. 1998. Overexposed: Organophosphate insecticides in children's food. Washington: Environmental Working Group/The Tides Center.
Zahm SH, Ward MH. 1998. Pesticides and childhood cancer. Environ Health Perspect Suppl 106:893.
[1] The USEPA requirements for registration may seem stringent: “Potential registrants must generate scientific data necessary to address concerns pertaining to the identity, composition, potential adverse effects, and environmental fate of each pesticide” (USEPA 2013). But most of the data is generated using a single substance in animals, an experimental design that is not able to model chronic health hazards accurately. Much of the research is sponsored by the company seeking registration and is not published in peer-reviewed journals. Most chemicals were grandfathered in under TSCA (Toxic Substance Control Act), and once registration is granted, chemicals are rarely re-reviewed, even given substantial evidence of harm.
[2] “Although correlations between algorithm scores and urinary levels were quite good (i.e., correlations between 0.4 and 0.8), exposure misclassification would still bias relative risk estimates in the AHS towards the null and diminish study power” (Blair 2011).